Chronic arthritis doesn't have to mean permanent pain. Discover how modern shoulder replacement surgery restores function and helps patients return to an active life.

Living with chronic shoulder pain can feel like carrying a weight that never lifts. Simple tasks like reaching for a coffee cup, brushing hair, or getting dressed become daily reminders of limitations.For thousands dealing with severe rotator cuff damage or shoulder arthritis,the path forward seemed bleak - until reverse shoulder replacement changed everything. This innovative surgical approach has transformed outcomes for patients who previously had limited options, offering renewed hope and restored function.

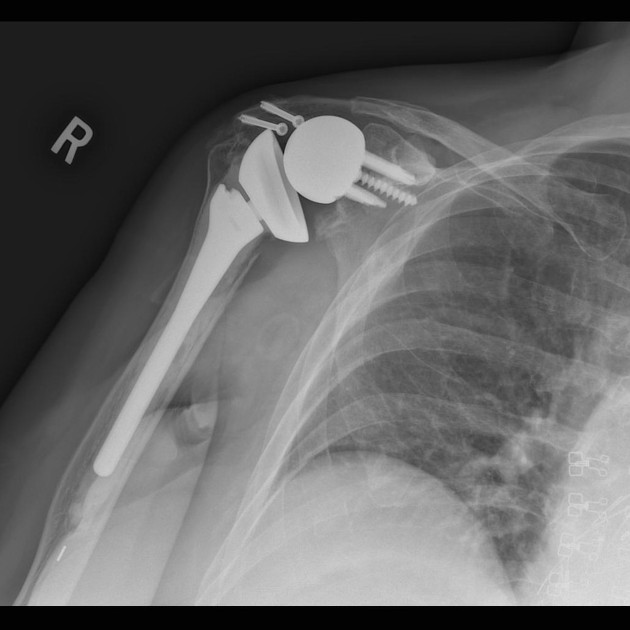
What is a reverse shoulder replacement? Unlike traditional shoulder surgery, this procedure flips the natural anatomy of the shoulder joint. The ball and socket trade places - the ball component attaches to the shoulder blade while the socket component goes onto the upper arm bone.This seemingly simple reversal creates a mechanical advantage that allows the deltoid muscle to compensate for damaged or torn rotator cuff – this is a specialised group of tendons that are unique to the shoulder joint. Their primary role is to centre the ball on the socket.
The technique addresses a fundamental problem that has plagued shoulder surgeons for decades. Traditional anatomical shoulder replacements rely on intact rotator cuff tendons to function properly. When these tendons are severely damaged or missing, conventional implants fail to provide adequate pain relief or restore movement. Reverse shoulder replacement surgery sidesteps this limitation entirely by redesigning how the shoulder operates.
The shoulder joint ranks among the most mobile joints in the human body, allowing an incredible range of motion in multiple directions. This mobility comes at a cost - the joint depends heavily on surrounding muscles and tendons for stability. The rotator cuff, a group of four tendons and their muscles, plays a critical role in keeping the shoulder stable while enabling smooth movement. When these structures deteriorate or tear beyond repair, the shoulder loses both stability, function and will eventually develop arthritis. Pain becomes constant, and even basic movements turn into struggles. Rotator cuff tears are incredibly common, occuring in up to 30% of people over 70.
Before this innovative procedure became available,patients with severe rotator cuff damage faced limited options. Many endured chronic pain with minimal relief from medications or injections. Physical therapy could only accomplish so much when the underlying structural damage was too severe. Traditional shoulder replacement failed these patients because the procedure design assumed a functioning rotator cuff. The development of reverse shoulder replacement filled this critical gap in treatment options.
The rise of reverse shoulder replacement represents one of orthopedic surgery's most significant advances in recent decades.According to research, the number of performed RTSA in the US has increased from 22,835 in 2011 to 62,705 in 2017. This growth reflects both expanding surgical expertise and proven success rates. Globally this shoulder prosthesis is now the predominant type used, in some countries by a factor of three times.
Studies from Johns Hopkins Medicine indicate that about 85-90% of patients who undergo this procedure achieve excellent pain relief. Beyond pain reduction, many patients regain the ability to perform activities they thought were lost forever. The procedure's success stems from its unique bio-mechanical design that leverages the strong deltoid muscle to power shoulder movement, even when rotator cuff function is compromised or absent.
Reverse shoulder replacement proves most effective for specific shoulder conditions. Ideal candidates typically include patients with:
• Massive rotator cuff tears that cannot be repaired
• Rotator cuff tear arthropathy (shoulder arthritis secondary to rotator cuff damage)
• Failed previous shoulder replacement surgeries
• Complex shoulder fractures in older adults
• Shoulder osteoarthritis (wear and tear arthritis)
Age plays a role in surgical planning, though it's not an absolute barrier. Most candidates are over 60, but younger patients with specific conditions may benefit. The key determining factors involve the extent of rotator cuff damage, bone quality, and overall health status rather than age alone.
Understanding the distinction between these two approaches helps clarify why each serves different patient populations. The choice between anatomic and reverse techniques depends entirely on the condition of the rotator cuff muscles.
The advantages extend beyond the impressive pain relief statistics. Patients typically experience significant functional improvements within months of surgery. Most regain the ability to reach overhead, perform self-care tasks independently, and return to recreational activities they enjoy.
The predictability of outcomes gives both surgeons and patients confidence. Unlike some procedures where results vary widely, reverse shoulder replacement delivers consistent improvements across diverse patient populations. This reliability stems from the procedure's fundamental design—by not depending on rotator cuff tendons, it avoids the main source of unpredictability that affects anatomical shoulder replacements.
Research indicates that approximately 85% of patients successfully return to recreational sports and physical activities after reverse shoulder replacement. Golf, swimming, fitness activities and even tennis can become possible again for many who thought their active days had ended. While contact sports are discouraged, the range of achievable activities surprises many patients positively.

While outcomes prove excellent for appropriate candidates, reverse shoulder replacement involves tradeoffs. Range of motion,particularly for reaching behind the back, may remain somewhat limited compared to a healthy shoulder. However, for patients whose alternative was chronic pain and severe disability, this limitation rarely diminishes satisfaction.
Recovery requires commitment. The rehabilitation process typically spans several months, with minor initial restrictions on movement followed by progressive strengthening exercises. Patients must work closely with physical therapists to maximize results and avoid complications.
This question misframes the comparison. Neither approach is inherently better or worse. For patients with healthy rotator cuffs and arthritis, anatomic replacement often delivers superior range of motion.However, for those with rotator cuff tears or damage, reverse replacement provides dramatically better outcomes than anatomic techniques could achieve.The procedure selection depends on individual anatomy and pathology rather than one being universally superior.
Understanding the recovery journey helps patients prepare mentally and physically. The typical timeline includes:
• First 6 weeks: Gentle range of movement and functional exercises
• 6-12 weeks: Progressive range of motion exercises under supervision
• 3-6 months: Active strengthening and functional training
• 6-12 months: Continued improvement and return to most activities
Pain relief often begins within days or weeks, while functional improvements accumulate gradually over the first year. Patience during rehabilitation directly correlates with final outcomes.
Implant longevity concerns anyone considering joint replacement. Research tracking patients for 10 years or more shows survival rates between 85-90%, meaning the vast majority of implants continue functioning well a decade after surgery. Factors affecting longevity include patient age, activity level, bone quality, and adherence to activity recommendations.
Younger patients may face higher revision rates over their lifetimes simply due to longer implant life expectancy and being more active. Ongoing advances in implant design and surgical techniques continue improving durability and longevity. Many patients enjoy decades of pain-free function from their reverse shoulder replacement.
Selecting an experienced shoulder surgeon significantly impacts outcomes. Surgeons who perform high volumes of reverse shoulder replacements demonstrate better results and lower complication rates.You can book a consultation and ask about surgical volume, complication rates, and the surgeon's experience with their specific condition.
Understanding all treatment options matters equally.Some conditions might respond to alternative approaches like physical therapy, injections, or arthroscopic (keyhole) surgery. Reverse shoulder replacement represents the optimal choice when conservative treatments fail and specific anatomical criteria are met. A thorough evaluation ensures the procedure is appropriate for the problem.
Reverse shoulder replacement has earned its reputation as a game-changer by delivering consistent, life-improving results for patients who previously had few good options. The procedure's unique design solves problems that stumped orthopedic surgeons for generations. While not appropriate for every shoulder condition, it provides remarkable benefits for the right candidates.
For those living with severe shoulder pain, loss of function, and diminished quality of life due to rotator cuff damage or arthritis,this surgical approach offers genuine hope. The combination of reliable pain relief, functional restoration, and long-term durability continues helping thousands of patients reclaim active, fulfilling lives. As techniques and implants evolve, outcomes will likely improve further, cementing reverse shoulder replacement's position as one of modern orthopedics' most important innovations.